Human papillomavirus (HPV) affects epithelial cells and has a particle diameter of 55 nm. A special feature is the proliferation of the epithelium of the skin, as well as the mucous membranes. At the initial stage, the pathogen usually affects the basal cells of the epithelium, penetrating them through microtraumas. Localized papillomas are usually found on the skin of the neck, armpits, groin and genitals (most often), oral mucosa and nasopharynx.
This virus can exist for many years without symptoms. For the detection of HPV, microscopic or molecular electron hybridization methods are used.
Types of human papillomaviruses
Humans have HPV, which affects mucous membranes and skin. Among the large number of papillomaviruses, there are species with low and high oncogenic risk. Oncogenic properties have been shown to be linked to the ability to incorporate DNA into the genome of human cells.
The virus is activated in 10-20% of cases. Depending on its type, it can lead to benign or malignant lesions. Some HPVs are not oncogenic. They lead to the appearance of genital warts and warts. The most common are HPV 6 and 11.
HPV oncogenes are those that have a high risk of developing cancerous lesions, especially in the cervix or anus. When it comes to the skin, HPV 16 and 18, as well as 5 and 8, which can lead to skin cancer, are more common. The most well-known form of cancer caused by HPV is cervical cancer. But men can also be infected with the papillomavirus, which in the worst cases causes cancer of the penis or anus.
Often women encounter HPV 16 - this is a form in which endosomal parasitism is observed, that is, outside the cell chromosome (benign). HPV 18 has a high risk of developing cancer - first benign tumors are formed, which after some time degenerate into cancer. Virions in this case have tiny sizes (up to 30 nm).
- neoplasms of the cervix;
- invasive or pre-invasive oncology.
- genital warts of the urinary system and genitals.
Infection characteristics

Human papillomavirus is highly contagious. It is usually spread through direct skin-to-skin or mucosa-to-mucosal contact with an infected person. For a genital infection, this most often occurs during vaginal or oral intercourse. Having a large number of sexual partners or other STDs (sexually transmitted infections) increases the risk. Indirect transmission through objects, contaminated clothing or bedding is also possible, but is quite rare.
In 7% of cases, transmission of the virus from mother to child can occur during childbirth, when the infection is active. The risk increases to 40% if infected with HPV 16 or 18.

Penetrating the epithelium, violating its integrity, papillomavirus infection promotes the growth of the lower layer of epithelial cells in the form of warts or warts. This form of the disease is contagious and quickly spreads to others. As a rule, warts and warts do not metastasize and often disappear spontaneously.
HPV symptoms
The incubation period lasts up to 9 months (average 3 months). HPV can be present in the body without any obvious symptoms. The virus can go undetected for months or years. Even at this stage it is contagious.
Skin warts usually appear in groups and increase in number when scratched. The two most common forms of papillomas are either grayish, hard, raised with a broken surface (common warts) or flat and reddish (flat warts). Warts appear on the soles of the feet or heels, grow inward and are therefore often painful.
- Genital warts. Pale or reddish nodules that often appear in groups and appear on the lips, vagina, penis, urethra, anal canal and rectum. They are highly contagious.
- Flat warts. They appear in the form of flat nodules and are mainly found in the female genitalia. They increase the risk of developing cancer.
- Giant warts (Buschke-Levenshtein tumors). They grow in huge formations, destroying the surrounding tissues. In rare cases, they can degenerate and lead to squamous cell carcinoma.
Infection of the mucous membranes in the upper respiratory tract is also possible. The conjunctiva of the eyes may be affected, resulting in pink stalks.
It is more difficult to identify an asymptomatic course, which the doctor can only see with the help of auxiliary means such as acetic acid (causes discoloration of the warts) or the microscope.
In addition, the virus can also settle in cells without tissue changes. Then they talk about latent infection, that is, the presence of pathogens, but without symptoms. Once infected, this phase can last from several weeks to several months.
Possible consequences
When infected, the viruses penetrate the cells of the skin and mucous membrane envelope, settle in the nuclei of cellular structures and multiply there. Typically, such HPV infections go unnoticed and heal on their own without consequences, since the immune system successfully fights the pathogen.
However, some types of HPV create skin changes called growths. Possible forms include genital warts or warts and papillomas, which may affect, for example, the face, hands or feet.
The tissue changes caused are mostly benign, but can also degenerate and lead to cancer. For example, cancer can appear decades after HPV infection. Cancer of the female external genitalia (cancer of the vulva and vagina), cancer of the anus, cancer of the penis, and cancer of the mouth and throat (tumors of the head and neck) are also possible.
Establishing a diagnosis

An examination for HPV infection is carried out in women as part of preventive visits to the gynecologist. During a gynecological examination, a smear is taken from the lining of the cervix, this is called a pap smear (cytological test). The resulting material is studied for tissue changes to determine precancerous conditions.
In addition, an HPV test may be performed, in which cellular material from a mucosal smear or tissue sample is tested in a laboratory for the presence of certain viruses. However, this only proves that the affected area is infected, but makes no statement as to whether tissue changes have occurred. Thus, an HPV test makes sense, especially when combined with a Pap test, and can help detect early cancer precursors.
If the test is positive, there is no need to worry, as infections do not always lead to cancer. Regular examination is recommended to detect tissue changes at an early stage. Conversely, a negative test result does not indicate whether there was a previous infection that the body successfully fought off.
For men, there is no screening in which the examination will be carried out regularly. If there is an underlying cancer, screening the tumor can determine whether HPV infection is behind the cancer.
Specialized DNA methods are also used in laboratory diagnosis, such as real-time PCR. Genital warts caused by HPV types 6 and 11 are easily detected during a gynecological examination.
How to treat human papilloma virus

In most cases, the disease does not require treatment because it goes away on its own and then the viruses are no longer detected. However, if this is not the case, the infection may last longer and persist for months or years.
To date, there are no methods of systematic influence on this virus that could completely destroy it. However, treating existing warts reduces the number of viruses, so in many cases the immune system can fight the remaining viruses and thus get rid of them. In some cases, the pathogens survive and can cause symptoms of the disease again and again.
- Plantar and genital warts can be treated with medications made with salicylic acid for topical application.
- Cryotherapy is also a method often used for HPV. In this case, the wart is burned with cold, using liquid nitrogen.
- Lasers or electrocautery are equally used methods.
For cancer caused by HPV, treatment is much more difficult. For cervical cancer, it is often recommended to remove the uterus, respectively the upper part of the vagina and the ovaries. This can be supplemented with radiation therapy to eliminate the possibility of recurrence. Other cancers caused by HPV are more often treated with targeted therapy, such as radiation or chemotherapy.
It should be remembered that the operation is not a radical solution, but only solves a cosmetic problem, since after removal the virus can remain in the surrounding tissues and the warts can appear again.
Prevention of infection

There are two vaccinations: a bivalent vaccine against HPV 16 and 18 and a quadrivalent vaccine against HPV 6, 11, 16 and 18. Vaccination is recommended for all young girls aged 14 years and older.
Vaccination does not protect against all types of HPV. Therefore, all women between the ages of 25 and 65, even if they have been vaccinated, are recommended to undergo regular Pap tests.
Early detection and complete removal of warts reduces the risk of disease. The effectiveness of using condoms to protect against the transmission of infection can significantly reduce the risk of developing this disease. The most promising way to prevent and treat the initial stages of the disease caused by this infection is a special multivalent vaccine.
Why plantar warts appear and methods of treatment
Warts are skin lesions that appear in the form of special round formations that protrude above the surface. They occur due to specific viruses.

These formations often cause physical discomfort due to their location. Even after treatment they tend to recur.
Types and reasons
There are many varieties of warts; they are classified according to certain characteristics:
- Simple. They appear on exposed parts of the body, hands, feet, face and scalp. They are usually not dangerous, but they are not aesthetically pleasing and can multiply quickly, affecting large areas of the skin. They are arranged as in "families".
- Plantarly. Their detection is done exclusively on the feet. It causes discomfort when walking.
The main cause is infection with the human papillomavirus, which affects the mucous membranes and skin.
Human papillomavirus
This is one of the most common viruses on Earth. Infection can occur in several ways:
- contact and household (through touch).
- sexual (genital, anal, oral-genital).
- in childbirth from mother to child.

The period of development of the disease ranges from several weeks to tens of years, this is explained by the fact that the virus may not manifest itself for a long time, but as soon as the immunity weakens a little, growths on the skin and/or mucous membranes immediately appear. The main danger of this disease is that some types of HPV are very likely to cause the formation of a malignant tumor (cancer of the skin or mucous membranes). To make sure that the disease will not lead to the formation of a tumor, it is necessary to undergo an examination by a doctor and not to self-medicate.
Symptoms and types of warts on the leg
A plantar wart appears as a callus-like thickening with a layer of the stratum corneum of the skin. It prevents walking and causes pain. The passive state is characterized by slow reproduction, not reaching the stratum corneum of the epithelium, so this state is not manifested externally.
The active state is characterized by the fact that the virus grows rapidly and, rising to the upper layers of the skin, manifests itself with many symptoms. Plantar ant is also called spiny ant, chicken wart. The virus enters through skin contact through cuts and abrasions in the outer layer of the skin:
- Initially, a small yellowish-gray papule with an uneven surface appears.
- Gradually, the small element becomes dense and acquires a dirty color.

From the inside, a plantar ant looks like fused nipples of different sizes with a pink tint. Extra capillaries form there, causing bleeding if you get warts.
Removal of plantar warts
It is worth treating a plantar wart if:
- There are painful sensations.
- The wart is bleeding.
- There were spots on it.
- The wart increases rapidly in size.
There are many treatment methods. One of them is cryodestruction. The meaning of the method is that the ant is exposed to liquid nitrogen at a temperature of minus 196 degrees. The area affected by the virus is iced and the wart is removed.
The usual and aggressive exposure method is used. With the aggressive method, nitrogen is applied for a few seconds longer, but this method is more painful. It is important to note that if a wart appears and exists for more than six months, then the effectiveness of cryodestruction is significantly reduced, and the meaning of such an operation, accordingly, also disappears.
After removing a plantar wart using liquid nitrogen, you should follow certain recommendations:
- the hive that remains at the site of the wart cannot be opened.
- To avoid mechanical damage, use a sterile dressing instead of a cast.
- Treat the affected area with 2% salicylic alcohol twice a day.
- try to prevent water from entering the affected area.
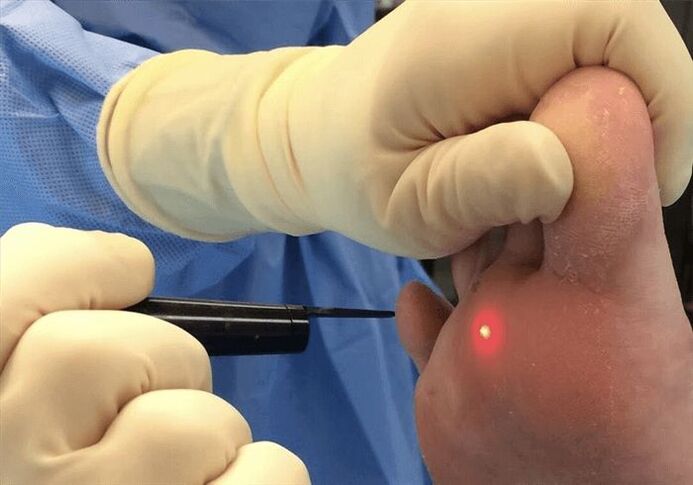
Another method is laser coagulation. This is one of the most common methods for removing warts. Most laser systems are equipped with a special cooling system. Thus, the procedure is done with minimal discomfort and does not allow inflammation, since the laser has antiseptic properties. Moreover, this is a non-contact method.
There are several ways:
- Carbon dioxide (CO2) laser. The treatment in this case is done using infrared light. The method is 70% effective, but the downside is that healthy tissue can also be damaged.
- Erbium laser. This treatment method uses a shorter wavelength, which reduces the chance of scarring after surgery. The efficiency is usually 75%.
- Pulsed dye laser. With this method of exposure, the primary destruction of the dilated capillaries in the warts and the stimulation of the immune system, which contributes to effective healing. The effectiveness of the treatment is about 95%.
After laser treatment, a crust forms on the affected area, which disappears on its own within seven to ten days. The recommendations for this method of treatment are the same as after exposure to nitrogen - avoid mechanical damage and water ingress.
The next way to remove warts is electrocoagulation. In this case, a high frequency current is applied to the wart. The treatment is performed under local anesthesia. Exposing a wart to high temperatures leads to the evaporation of cells affected by the papilloma virus. Another advantage of this method is that cauterization of the blood vessels prevents bleeding. After surgery, a crust forms on the affected skin area, which disappears within 7 to 10 days.
A plantar wart can be treated with immediate surgery. In this case, the excision is performed under local anesthesia and then sutures are applied. After the operation, the doctor will prescribe certain recommendations. Thus, it is recommended to prevent water and soap from entering the affected area, not to tear the resulting crust and treat the affected area with an antiseptic for the first 7-10 days.

For each type of operation there are certain contraindications. Thus, it will be impossible to perform the function if the following occurs:
- pregnancy;
- Diabetes;
- malignant tumors in the body.
- infection and inflammation around the wart;
- exacerbation of herpes;
- increased temperature.
If your blood pressure is high, the procedure should also be postponed.
Treatment of warts without surgery

People often wonder how to remove a plantar wart without surgery. To do this, you can use medicinal ointments and solutions.
Basically, these ointments have the following effects:
- anti-inflammatory;
- antiseptic;
- immunomodulatory;
- antiviral;
- antifungal.
In addition, it may contain vitamin E, which also has a positive effect on treatment, since vitamins generally strengthen the body and reduce the risk of relapse.
It is important that these products are used for isolated and shallow plantar warts. In addition, if side effects occur, it is necessary to wash off the drug with plenty of warm water and immediately seek help from a doctor.
So, it is possible to treat warts, there are many ways to do this, but you should not do it without first consulting a doctor, so as not to harm your health. In addition, self-medication is strictly prohibited if the attending physician prescribes contraindications.
Treatment of papillomas on the body
Hardware methods
Modern material methods for the treatment of papillomas make it possible to get rid of them and prevent the development of a relapse of the disease. The most commonly used methods are:
- Cryodamage is the destruction of plants by exposing them to low temperatures.
- Electropexy is the cauterization of formations with electric current, the power and frequency of which is selected depending on the size, type and density of the papilloma.
- Laser removal. The type of impact is clear from the name. The procedure takes no more than 15 minutes and helps to get rid of unpleasant growths forever.
Pharmaceutical treatment
Among the drugs used are Celandine preparations, castor oil, pencil lapis, Sani Skin and Dermavit.
They demonstrate varying efficacy and do not prevent disease recurrence. The main disadvantage of drug treatment for papillomas is the frequent development of allergic reactions.
Prevention of papillomas
In order to avoid developing growths and to avoid infection with human papillomavirus, you should:
- Use barrier contraception during intercourse.
- Follow the rules of personal hygiene and use only individual towels, soap and toothbrush.
- When visiting public baths, do not neglect to wear rubber shoes.
You should also normalize your daily life, eat a balanced diet, give up bad habits and avoid stressful situations. These factors are not the cause of the disease, but they can cause its development if the virus is already present in the body.














































































